Education on
Cardiac Continuum
Patient Education
(CV Risk Awareness and More)
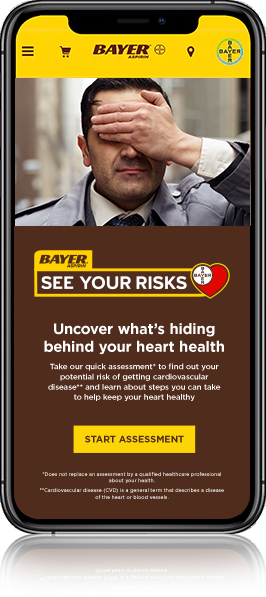
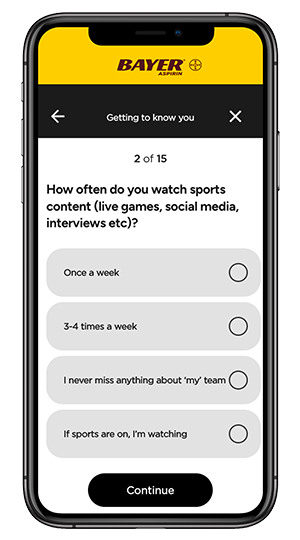
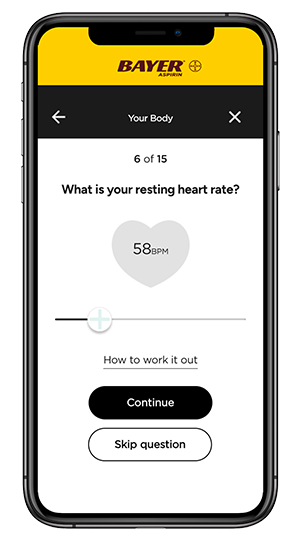
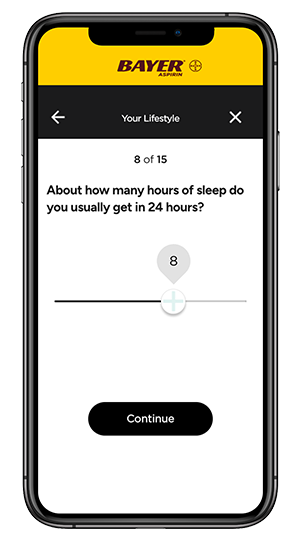
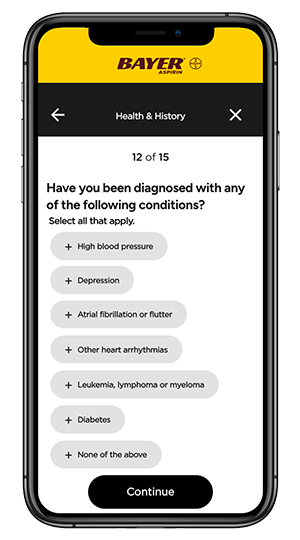
NEW! Bayer® Aspirin Heart Risk Assessment—a valuable tool for patient education about awareness of CV risk factors
- An evidence-based patient self-assessment
- Created and informed by expert cardiologists, this reflects well-established risk factors*
- Can help patients understand their potential risk factors for cardiovascular disease (CVD)
- Asks 13 questions and educates patients on whether they are lower, average, or higher risk† based on their risk factors over a 10-year period
- Allows patients to be more prepared for your conversations
*This assessment, developed by Huma Therapeutics (“HUMA”) and Bayer, is based on data from 466,052 participants in the United Kingdom recruited from 2006 to 2010. It estimates a patient’s 10-year risk of CVD by comparing their answers with the research population. The research is published in the European Heart Journal—Digital Health. Patients are informed that the assessment does not replace an assessment by a qualified healthcare professional.
†Compared with the population researched.1
Some questions your patients may ask you after using the tool include:
- What is my risk for a heart attack or stroke?
- What are the warning signs or symptoms I should watch out for?
- What can I do to lower my risk of heart disease and stroke?
- What is my blood pressure? Is it at a healthy level?
- What is my blood cholesterol? Is it at a healthy level?
- What is my blood sugar? Is it at a healthy level?
- What is a heart healthy exercise plan for me?
- What is a heart healthy eating plan for me?
- Are there any nutritional supplements that would help support my heart health?
Patient Discussion
(Secondary Prevention)
Relevant Publications
(Journal Articles, Guidelines, and More)
Practice Education
(Videos and More)
References: 1. Dolezalova N, Reed AB, Despotovic A, et al. Development of an accessible 10-year digital cardiovascular (DiCAVA) risk assessment: a UK Biobank study. Eur Heart J. 2021;2(3):528-538. doi:10.1093/ehjdh/ztab057 2. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. doi:10.1016/j.jacc.2014.09.017 3. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. doi:10.1016/j.jacc.2012.11.019 4. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. J Am Coll Cardiol. 2012;60(24):e44-e164. doi:10.1016/j.jacc.2012.07.013 5. Kulik A, Ruel M, Jneid H, et al. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation. 2015;131(10):927-964. doi:10.1161/CIR.0000000000000182 6. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. Circulation. 2016;134(10):e123-e155. doi:10.1161/CIR.0000000000000404 7. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Circulation. 2011;124(4):489-532. doi:10.1161/CIR.0b013e31820d8d78 8. Bushnell C, McCullough LD, Awad IA, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(5):1545-1588. doi:10.1161/01.str.0000442009.06663.48 9. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-2236. doi:10.1161/STR.0000000000000024 10. Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849-1860. doi:10.1016/S0140-6736(09)60503-1 11. Saini SD, Fendrick AM, Scheiman JM. Cost-effectiveness analysis: cardiovascular benefits of proton pump inhibitor co-therapy in patients using aspirin for secondary prevention. Aliment Pharmacol Ther. 2011;34(2):243-251. doi:10.1111/j.1365-2036.2011.04707.x 12. Jones WS, Mulder H, Wruck LM, et al. Comparative effectiveness of aspirin dosing in cardiovascular disease. N Engl J Med. 2021;384(21):1981-1990. doi:10.1056/NEJMoa2102137